A Second Heart Attack Almost Killed Me: How I Survived
The story of how I went from healthy to heart failure in two years, and how I hope to help other heart failure patients and their support team.
Welcome to My Heart Failure Life
Welcome to My Heart Failure Life, a newsletter about my journey with heart failure—written for fellow HF patients and the people who love and support them.
I share my firsthand experiences with cardiac events, medications, tests, ER visits, symptoms, and the times I knew to call 911. I also break down medical jargon and the realities of living with heart failure in a way that’s honest, practical, and relatable.
What I don’t do is give medical advice—I’m not a doctor, just someone navigating this road like you. If that sounds helpful, subscribe today and get every post delivered straight to your inbox—for free. You can unsubscribe at any time. And if you know someone who could benefit, feel free to share!
It Began Without Warning
I don’t remember the worst of it.
One moment, I was standing in the hallway outside my office after conducting a funeral, dismissing a slight chest discomfort as stress. The next, I was waking up in a hospital bed at Duke University Medical Center, breathing with a ventilator, tethered to machines, my body battered by a battle I had no memory of fighting.
But the people around me remembered. My wife, Debbie, who had called 911 as I lay on the couch in my office. The paramedics, who worked frantically to stabilize me. The emergency room staff, who fought to bring me back from the edge—three times. The cardiologists, who struggled against arteries so clogged that the usual procedures barely worked.
This second heart attack wasn’t just worse than the first—it was catastrophic.
I had survived one heart attack already, back in November, 2021. That time, I had textbook symptoms: crushing chest pain, radiating arm discomfort, a desperate call for help. But despite the severity, I remained conscious, made it through the hour-long ambulance ride, and underwent an emergency catheterization to have three stents placed. I recovered. I adapted. I thought I had dodged the worst.
But heart disease isn’t just a single event—it’s a lifelong condition. And on September 9, 2023, it came for me again, this time with no warning and no mercy.
No Warning, No Mercy
That Saturday morning, I felt fine. The funeral I conducted was taxing, but I had done this many times before. People even commented to Debbie afterward that I seemed engaged, energetic, and completely myself. There was no hint—no fatigue, no dizziness, no discomfort—to suggest what was coming.
Then, as I stepped into my office after the service, a slight chest pain started. At first, I dismissed it. It felt like the angina I had grown used to—manageable, familiar. But then it escalated, and fast. Within moments, I knew. This was different. This was bad. This was worse than my first heart attack.
That’s when Debbie called 911.
I don’t remember much after that. The first paramedic came in, and I must have spoken to him. But I have no memory of being placed on the stretcher or taken out of my office. I only know what happened next because others have filled in the gaps.
A Fight for Survival
The ambulance ride to the hospital in Danville, Virginia, took about 15 minutes. When I arrived at the ER, I was in full cardiac arrest. My heart stopped three times. Each time, the medical team fought to bring me back. My wife, sitting in the waiting room, heard nothing. For hours, no one came out to update her because my condition was too critical. Every moment was spent trying to save my life.
The doctors rushed me into the catheterization lab, where they faced a grim reality. The same arteries that had been stented in my first heart attack were now completely blocked again—this time even further back into the main artery. The procedure to reopen them was complicated, nearly impossible. The doctors struggled to get through the blockage, changing tools mid-procedure. When it was finally open, they placed new stents. But even then, I was not stable.
I had already endured the full force of cardiogenic shock—when the heart fails so completely that it can no longer pump enough blood to sustain life. I was connected to every form of life support available. And then, the doctor told my wife something chilling:
“We don’t know how this is going to turn out, but if you’re a praying person this is the time.”

The Long Road to Duke
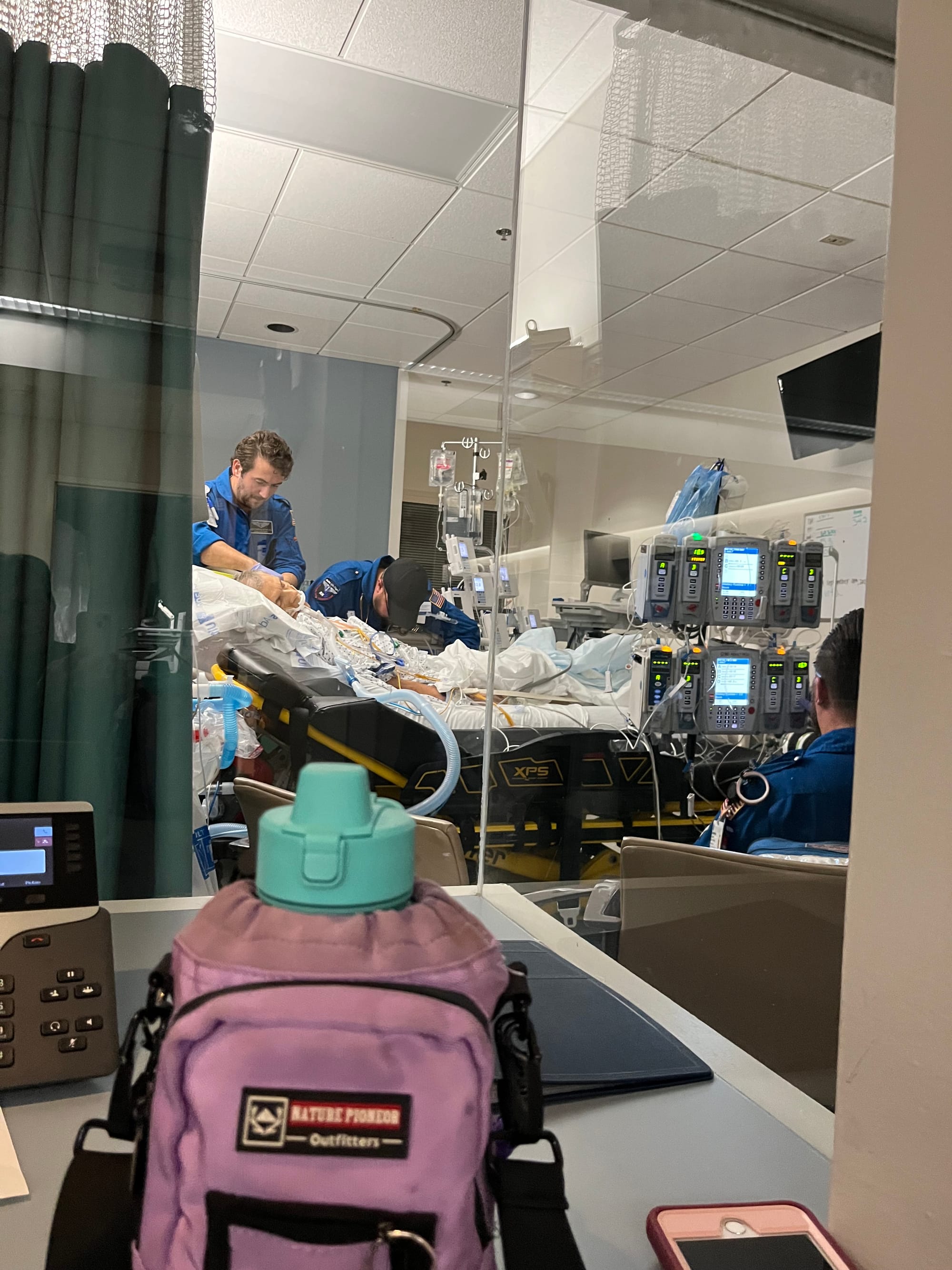
Immediately after the stents were placed, I needed to be transferred to Duke University Medical Center, where more advanced care was available. Normally, they would have flown me by helicopter. But that night, a storm rolled in, grounding all flights.
Instead, Duke sent their rolling ICU—a massive, high-tech mobile intensive care unit designed to keep critically ill patients stable in transit. Before they could move me, the team had to carefully switch me from the hospital’s life support to their own systems, making sure I stayed alive in the process. The trip wasn’t fast. It wasn’t a mad dash down the highway. It was slow, methodical, careful—because every moment, I was being treated as if I were still in an ICU bed.
We arrived at Duke around 5 a.m. Sunday morning. I remember none of it.
For the next two days, I remained unconscious, completely unaware of what had happened to me.
Waking Up to a New Reality
On Tuesday afternoon, I surfaced. A voice was calling to me, telling me to squeeze my wife’s hand. Then to squeeze the doctor’s hand. Right hand, then left. They were checking for brain damage.
I was in a hospital room, unable to move, hooked up to a ventilator, and surrounded by tubes and machines. I was confused and angry. I didn’t know where I was or how I had gotten there. I had no memory of the heart attack, the ambulance, or the long fight to keep me alive. Slowly, Debbie and the doctors began to explain what had happened.
When I pressed them, the cardiologists told me what they thought had caused it: six months earlier, I had been taken off Plavix, an anti-platelet medication which slows blood clotting. In preparation for a prostate biopsy, I also had stopped taking a daily baby aspirin at the urologist’s instruction. Being off both anti-platelet meds at the same time was the only apparent explanation for my LAD artery re-clogging completely, but even that was a guess.
Meanwhile, my body was struggling to stabilize. My blood pressure fluctuated wildly. My heart rhythm was erratic. My electrolytes were dangerously imbalanced. Every hour brought another adjustment—another IV drip, another round of medication, another check to see if my body was strong enough to survive.
By Wednesday, physical therapy began. At first, all I could do was sit on the side of the bed. The exhaustion was overwhelming. But by Thursday, I had managed to walk slowly down the hallway with assistance a couple of times. That was when the doctors moved me out of intensive care and into a step-down cardiac unit.
I was improving. The worst was behind me.

A Second Chance at Life
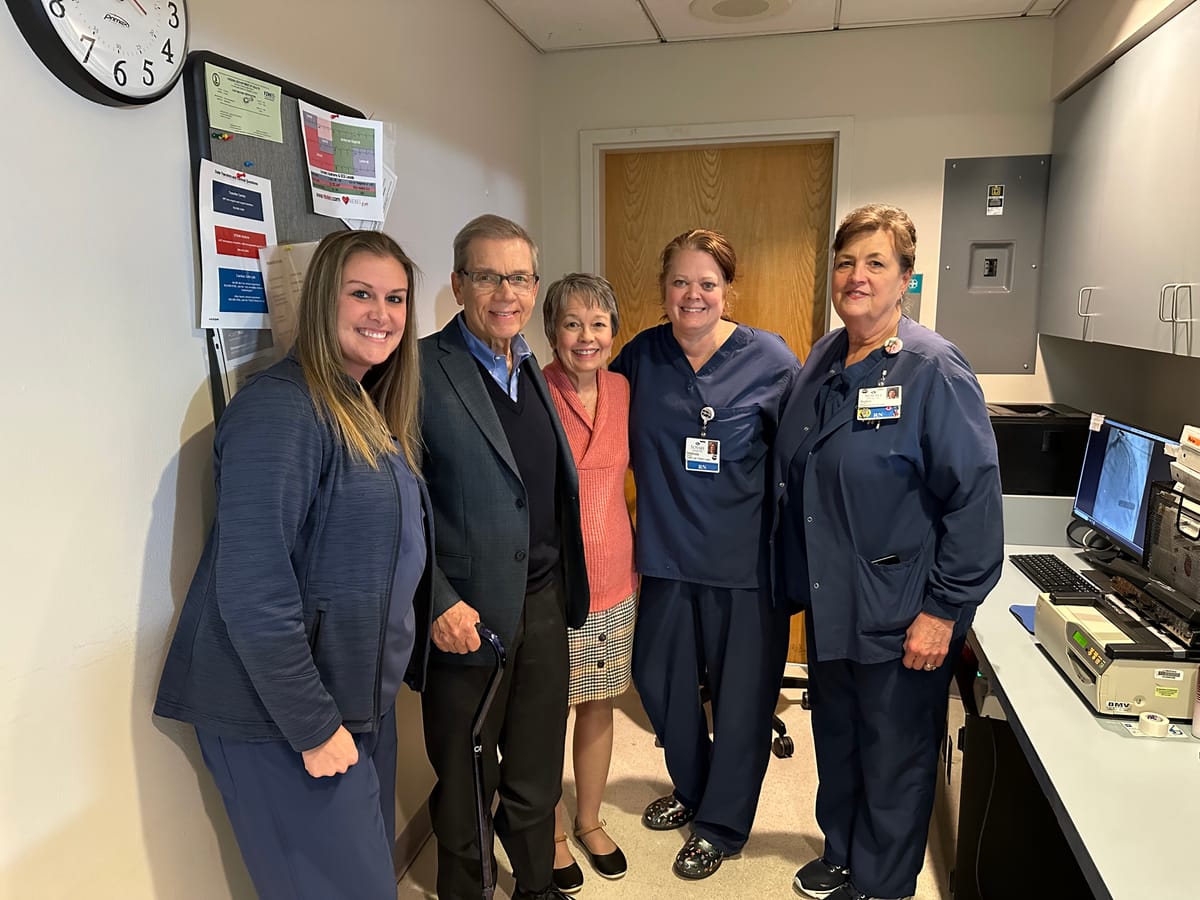
The team at Duke started calling me “the miracle man.” I had survived a heart attack that should have killed me—many times over.
By Saturday, I was stable enough to go home. Seven days after arriving at Duke on the brink of death, I was wheeled out of the hospital, frail but alive.
But I wasn’t the same.
This second heart attack had left its mark. Unlike the first, this one had permanently damaged my heart. According to the American Heart Association, heart failure is diagnosed as one of four stages – A through D. When I was discharged, I was classified as a “Stage C heart failure patient”—meaning my heart’s ability to pump blood had been severely weakened. My recovery this time would be longer and harder – my limitations, more significant.
And yet, I was still alive. I was still breathing, still walking, and eventually still capable of sitting at my desk to write these words. One year and four months have passed since that life-changing experience.
I knew then what I know now: every day is a gift.

That is my story, at least the main parts of it. And, that’s why I’m writing this newsletter. Because from my first heart attack, through the second one, and right to this present moment, this journey has not been easy. But I've learned a lot and I'm happy to share my experiences to help others.
Next time, the main article will be shorter, and I’ll add some new features like low-sodium recipes, and I’ll clarify some medical jargon. Join me here and spread the word. Together, those of us living with heart failure, and our support team, can become a community that informs, nurtures, and encourages each other. See you soon! -Chuck



